Work
Case Study
For inpatient therapies, hospital transparency data is rich with commercial insights and applications-if you know where to look. Learn how Payer Sciences turned disparate, difficult-to-decipher hospital pricing data into a communications piece that turns perceived financial risk into net cost recovery.
White Paper
For inpatient therapies, hospital transparency data is rich with commercial insights and applications-if you know where to look. Learn more about how the insights from this data can shape discussions between manufacturers and hospitals about coverage and reimbursement.
Trends
Traditional promotional mix models include personal interactions, samples, leave behinds, non-personal messaging, and more. But is it time to expand your field of view to include key market access efforts? Read more to see how a comprehensive mix model analysis can benefit you.
White Paper
Payers act as gatekeepers who decide which drugs to cover and how to cover them. Each payer has their own specific rules for different drugs, which they apply and enforce in unique ways. Learn how applying a Gini score can help you make sense of this variability and guide strategic decisions to achieve your access goals.
Trends
Fact: 78% of physicians are employees of hospitals, health systems, and corporate entities. So the potential to prefer one treatment option over another could rest with the physician or with their employer. Payer Sciences has a unique method to analyze health systems’ influence on prescribing habits to help strategically target marketing resources. Read more to see how it can benefit you.
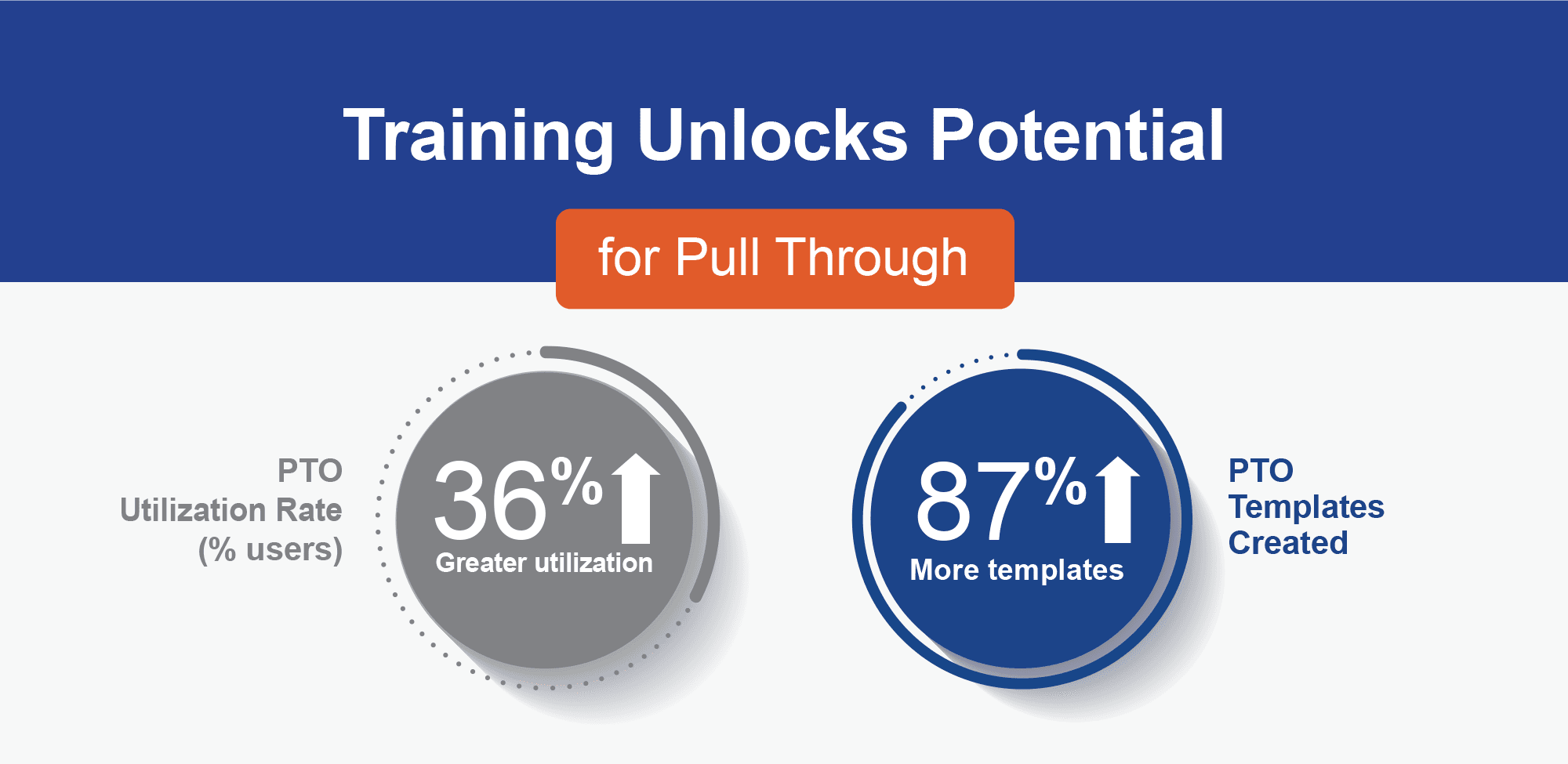
Case Study
Learn how Payer Sciences helps clients improve the effectiveness of their sales force by maximizing the usage and impact of the Pull Through Optimizer through education and training.
Case Study
Learn how Payer Sciences translated health economic data into clear and compelling messages. Read on to see how a FDAMA 114 presentation resonated across the IDN ecosystem.
Case Study
Learn how Payer Sciences helped a client keep messaging top of mind with consistent and frequent exposure wherever key decision-makers consumed media. Read on to see how the results spoke for themselves.
Data Story
The forming of physicians and other healthcare stakeholders into organized provider groups or OPGs is changing the way prescribing decisions are made. Learn how dramatically the landscape has changed, and what pharmaceutical marketers need to know to optimize strategies and tactics for their brands. Hint: The answers lie in the data.
White Paper
Payer contracting models traditionally rely on a top-down analysis which leaves one important question unanswered: How will a change in coverage position impact net revenue on a prescriber-by-prescriber basis? Learn about how our bottom-up model answers that question and more.
Case Study
Pull through is often disregarded in highly restrictive categories. Read about how we helped our client correct coverage misperceptions and increase volume.
White Paper
Setting a new specialty drug price is a daunting, high-stakes game. We think it’s time to reengineer the pricing decision process to include a variety of inputs. Learn more about how our disciplined approach helped our client establish an optimal price.
Case Study
Learn how Payer Sciences used our market access experience and network to help a client locate elusive gene therapy stakeholders for critical market research.
Case Study
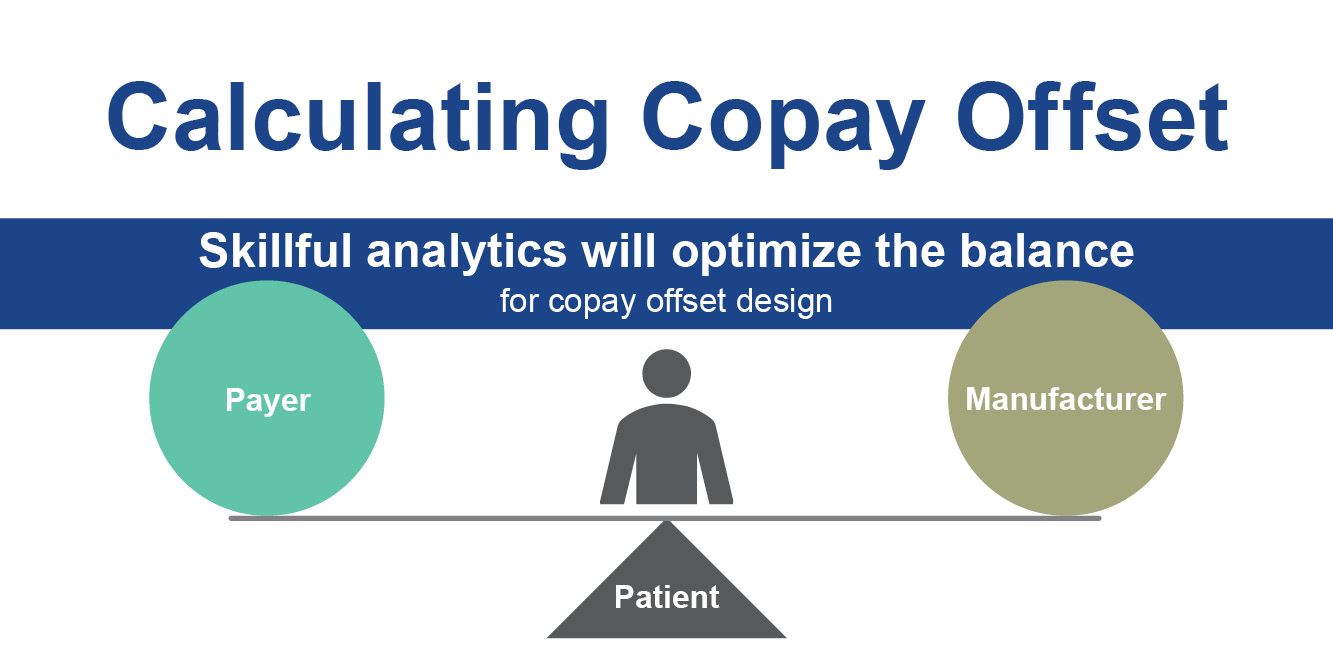
Read about how we helped a client calibrate and construct a copay offset program that ensured patient access without breaking the bank.
White Paper
For each prior authorization criterion a payer creates, your forecasted revenue bucket can spring a leak. Point of care staff armed with the right tools can better navigate obstacles and stop the leaks. Learn the 4 steps to effective access navigation.
Case Study
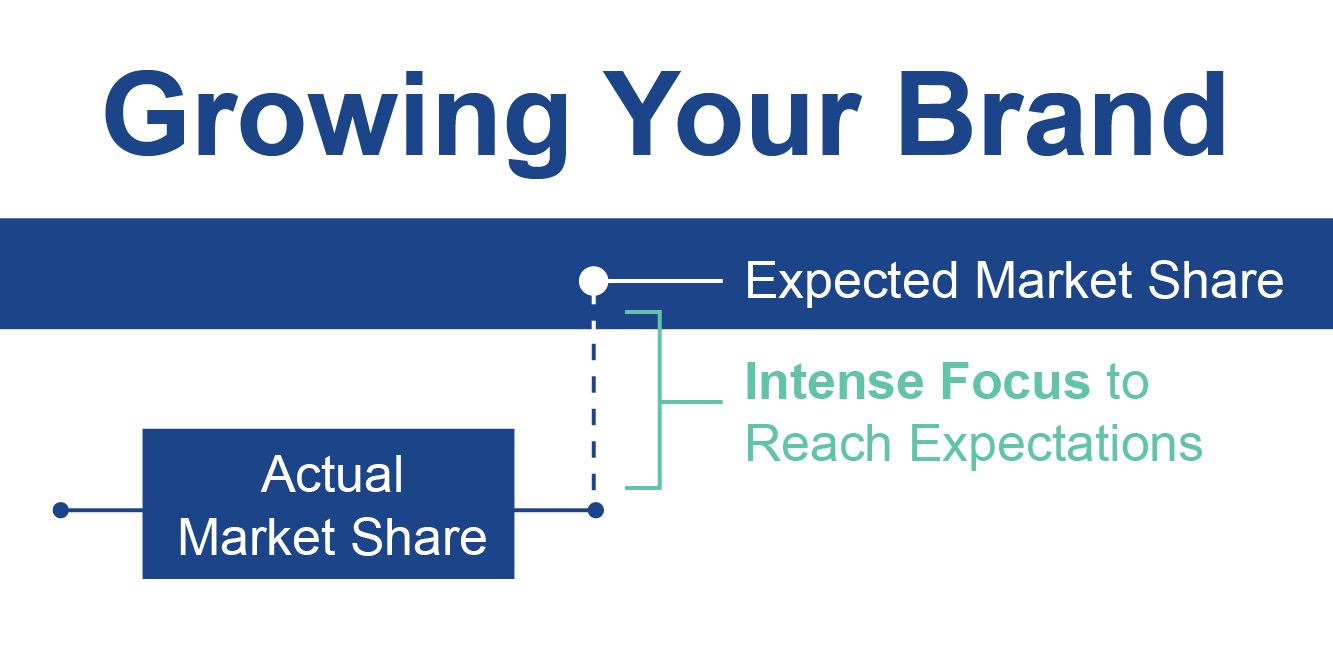
Before investing resources in brand share growth, it is crucial to gain a deep understanding of unique coverage environments at the individual HCP level. Learn how we can help.
Case Study
Read about how we helped a client by taking a unique approach to market segmentation that helped prioritize payers with the highest potential to restrict access and inform more tailored messaging.
Case Study
Read about how we helped a product vulnerable to generic substitution secure unrestricted access at launch, achieving its 90% coverage goal.
Case Study
Learn how, even with good coverage, relevant prescriber-specific messages can lead to increased sales representative confidence, increased HCP confidence, and 18% greater market share growth.
White Paper
Today, between 40% and 70% of healthcare providers are affiliated with an IDN or a provider network. But how do you know which to target? Learn how the right data analytics can disentangle the sources of influence to provide direction.